Human Rights and Health in Latin America
Socio-Cultural Reflections in Epidemiology
Development strategies that attempt to make improvements in the lives of the rural poor without addressing the underlying structural causes of poverty serve to deflect attention away from the real needs of impoverished communities. (Linda Green, Medical Anthropology Review, 1989)
Anthropologists, involved as we are with trying to understand the lives of people within their local worlds must be poignantly aware of the growing pauperization of the world and of the global forces which affect the everyday lives of people in the local communities we study. This is particularly pertinent for those of us who are concerned with issues of health and the various forms of human suffering, as we try to understand how best to assist local populations.
In 1974, Vincente Navarro spoke methaporically and dramatically but, I believe, not incorrectly, when he stated that the equivalent of twenty nuclear bombs explode every year in Latin America without making a sound. From all accounts, they are more numerous today. There is violence in the world, in all parts of the world, and quite clearly so in Latin America and the Caribbean. Civil wars, homicide from a whole range of motives, torture (whether state sponsored or not), rape and a pervasive climate of fear in the lives of all too many (100s and 100s of thousands of too many) have been a part of recent and current Latin American history. In a country such as Colombia, the national homicide rate is said to be considerably higher than in New York City. These human rights abuses quite clearly explain a great deal of the epidemiological–physical and mental health–patterns of people’s suffering in these countries (Desjarlais, et al, 1995).
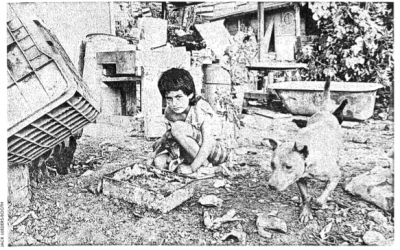
Structural adjustment policies are enforced on most developing countries. We are told, however, that this is “structural adjustment with a human face,” I am not convinced. Or rather, the evidence I read increasingly convinces me that this human face is not the smiling child’s face we see on the cover of books, but rather a crying face–the crying face of a child in misery.
The strength of anthropology is that we deal with “human faces,” we come close to the everyday lives of people–the specific, the local–and we depict (and expose) this local world, to ourselves, back to those we study, and, perhaps more importantly, to a more general public, including policy makers…..
It is not innovative for me to, once again, strongly urge that we focus on the inter-connections between the local worlds of the human faces and the global forces which very directly affect individual lives. But it bears repeating that we must constantly inter-relate the immediate and local with the global and pervasive if we are to truly understand why things are the way they are for the many, relatively small, groups of people among whom we work as “stranger and friends.”
This does not mean we should forego our strength–our involvement with local worlds in favor of the global/macro. The sources of the impetus for change are many and are often rooted in specific, local community-based activities. We must do both: we must ring the alarm bells, make the connections, point to the overwhelming forces and the overall statistics, as well as “show” the human faces.
Though not to be forgotten, the focus must shift from specific vectors and the so-called unhealthy behaviors of people, to examining the total condition of people’s lives–the context (as anthropologists emphasize) in which people have to live their everyday lives.
It is not particularly fashionable to speak of social pathologies when discussing health patterns, especially for marginalized groups. People’s eyes glaze over, and they throw their hands up in despair, when “poverty” is wheeled out as the underlying, root cause of disease. The problem, then, becomes too overwhelming, the required tasks too difficult. But, though difficult, the evidence for such a connection–for the social and human rights roots of disease–is inescapable.
What is some of the evidence in terms of the specific situation in Latin America?:
In the past 20 years, the health indices in Latin America have improved, and some countries have promoted social welfare as well as immunization programs and improved health services which have been quite effective. But differences exists within the region–with Costa Rica, Chile and Colombia doing quite well, while Bolivia, Haiti and Guatemala continue at the lower end of the scale. What we must also keep in mind, however, is that traditional indicators of health and well being, such as infant mortality rates, are not always the best measures of the increased suffering experienced by a growing proportion of marginalized people.
While maintaining that the most significant health risk factors are socio-economic and a matter of obtaining and ensuring basic human rights, inappropriate health services are also accountable. Unnecessary services, usually involving the use of expensive, sophisticated health technologies, consume one-fourth to one-third of the region’s $40 billion annual expenditure on health care. These services have little relevance to the most pressing needs of Latin America’s people. The balance between primary care and more complex services was inappropriate before the (economic) crisis, which appears to have made it still worse. As a result, around 700.000 deaths occur each year that could have ben avoided if the resources already available in the region were better allocated and utilized.
More important than the differences between countries are these differences within countries–largely a result of what can be called “functional apartheid.” During the years 1980 to 1991 inequality between the top sector and the rest of society has particularly increased in Argentina, Mexico, Guatemala, Venezuela, Brazil and Peru but has decreased in Costa Rica, Colombia and Chile (WB, 1995:105). The Zapatistas have called world-wide attention to the dire situation of the majority of the people of the State of Chiapas which, according to UNDP, has a Human Development Index (HDI) of 77 compared to one of 107 for the most affluent Mexican state of Leon. The disparities within Brazil are even worse. According to the UNDP: “The socio-economic indicators in North-East Brazil point to the potential for considerable trouble. The region lags behind the more prosperous South in every respect: the disparity between the two regions is 17 years in life expectancy, 33 percentage points in adult literacy and $2,000 (40%) in real GDP per capita. These disparities are much greater than those between Mexico’s state of Chiapas and the national average, and the recent trouble there should serve as a timely warning for policy-makers elsewhere” (UNDP, 1997).
By and large, anthropologists working within public health, and in collaboration with epidemiologists, have concentrated on the significance of cultural factors in explaining epidemiological patterns and in promoting successful public health interventions. In the most negative sense anthropologists have been used, as some where by colonialist earlier in this century and in the last, to find the culturally appropriate buttons to push to market preconceived “effective and necessary” public health interventions. In a more positive light anthropologists have been interpreters and intermediaries ensuring that public health interventions were mutually agreed upon and culturally appropriate.
Cultural patterns or practices do, of course, influence disease patterns–culturally sanctioned diets, roles for women, and the like all imply certain health risks or protection. Similarly, anthropologists’ concerns with the importance of understanding such concepts as the hot/cold dichotomies and the importance of “balance,” so prevalent for many groups in Latin America, have also enhanced public health efforts and patient-doctor relationships–the alliances with both individual patients and communities. Other contributions have been in relation to the health impact of the stresses of immigrant and refugee populations and the relationship between degrees of acculturation and health. Such work has obviously been of great significance and continues to be of importance.
But our concern must also include human rights and socio-economic (class) issues.
Navarro’s earlier point was that violence is not always direct or overt–it is also covert and silent. It is the violence resulting from the structure of de-facto apartheid (of “otherness,” “segregation”)–and whether such apartheid is official government policy or “only” functional makes little difference to those for whom it is a fact of their everyday lives.
A medical or public health program of any positive consequence, whether in Latin America or elsewhere must focus on, and grapple with, the national and international crisis which afflicts us all, and examine the root causes of inequity and the growing pauperization of the world. Our health–“theirs” and “ours” (which are intertwined)–depends on it.
Spring 1998
Kristian Heggenhougen is Associate Professor of Medical Anthropology at Harvard Medical School and Associate Professor of Population Sciences at the Harvard School of Public Health.
Related Articles
The Social Agenda in Latin America
If the 1980s were the era of economic policy reform in Latin America, the 1990s have become the era of social sector reform. Indeed, a consensus is now forming that delivery of health care…
A Mellon Update
More than 23 Latin American archives and libraries from Mexico to Rio de Janeiro have received grants from the Andrew W. Mellon Foundation to upgrade or preserve their facilities. The…
From Havana to HUD
Kennedy School Assistant Professor Xavier de Souza Briggs, who took a group of 17 graduate public policy students on a one-week study tour of Cuba last year, has now embarked on…