Diet, Poverty, Lifestyle and Health
A Conundrum for Latin Americans de la Sartén al Fuego?

Colombian children meet Father Fernandez’s plane with its flying health team.
The old pandemic which persists today
On a summer day in the early 1970’s two Harvard Medical students boarded a small plane in Turbo, Antioquia, Colombia and flew to an isolated community in the northeast of the province. They were part of an ad hoc medical mission organized by Father Fernandez, a Jesuit priest who indulged both his vocation of ministering to the poor and his love of aviation by flying health teams into isolated communities. The students, based at a small hospital in Apartadó, were serving two-month clerkships as participants in what was then a unique fourth year elective: “Medicine 518: Rural Medicine and Nutrition in Latin America” offered by the Department of Nutrition at the Harvard School of Public Health. Both students had learned medical Spanish in an intensive language program offered as part of the elective.
Although village children were familiar with Father Fernandez’ plane, they had never seen an automobile since there were no roads into the area. The visitors made their way to the small health post, now closed, but previously staffed by a practical nurse who had left several months earlier and not yet been replaced. As the village priest, the deputy mayor and other community leaders greeted the visitors, a man walked into the center of town with a wooden chair strapped to his back. Pedro Miguel, a sad four-year-old pale little boy with a very swollen face had been sitting on the chair for close to five hours. He had been ill for two weeks with mild diarrhea, weakness, loss of appetite and progressive swelling of the legs, eyelids and then the whole face.
During the previous week Pedro Miguel had spent most of the time in his cot, refusing food except for small amounts of potato and diluted soup. The swelling progressed, alarming his parents who brought him to Father Fernandez because they knew that “swelling came before death”. Pedro Miguel had been sick in the past with chicken pox, measles and many colds and episodes of diarrhea “like all children get”. He had been immunized once, although not the required three times. According to his father, Pedro Miguel was not a good eater. His diet consisted of corn porridge, arepas (corn bread), small amounts of beans and potato-based soups and almost no animal protein. Pedro Miguel’s parents were in their thirties. They farmed a small plot of land to which they did not have title where they grew corn, potatoes and a few vegetables. They kept two hens but the eggs were usually sold. Neither parent had finished grammar school.
Pedro Miguel’s pulse was 100. He was pale and his nail beds were white, a finding that was not given enough importance at the time. His hair was thin and could be easily plucked. The abdomen was soft but somewhat distended and the liver was large. Edema was massive over his face, including lips and eyelids; he could hardly open his eyes. The students were well trained to focus on Pedro Miguel’s diagnosis and treatment, but that was the tip of the iceberg. They had much to learn about the submerged portion of the problem, the web of indirect causes of Pedro Miguel’s life-threatening plight that would be impossible for them to cure.
The students reasoned that the swelling was due to low concentrations of albumen, a protein produced by the liver that is largely responsible for maintaining the osmotic pressure that reabsorbs fluid from the tissues back into the circulation. The likely diagnosis was kwashiorkor, or severe protein malnutrition which is usually the result of a diet chronically deficient in good quality protein accompanied by severe infection. They reasoned that Pedro Miguel was anemic because of his pallor but the severity was underestimated, perhaps because our diagnostic skills were blunted by technology available in Boston. The students knew that children with kwashiorkor have a 50% chance of dying even if admitted to a hospital for treatment.
The nearest health facility was more than one hour away by air and days away on foot. The boy was flown to Medellín, the capital of the province. As the small plane climbed over 15,000 feet to cross the Andes, Pedro Miguel became unconscious and had a seizure. Belatedly, we realized that the pale nail bed had not been taken seriously enough: he was suffering from critical lack of oxygen in the brain, the result of altitude (the cabin was not pressurized) and anemia far more severe than had been assumed. The pilot agreed to fly the canyons at a lower altitude and the boy looked better. When the plane landed in Medellín he was awake. The students drove him to the main public hospital where the resident physician in charge of the Emergency Department turned them away: he had two beds available and two dozen critically ill children in the waiting area. He suggested that they take care of Pedro Miguel at home and bring him back on Monday. Although sympathetic, he saw little sense in flying children with kwashiorkor to the University Hospital: Pedro Miguel should have been taken to a local hospital what he did not say was that local hospitals were underutilized because people knew that they were understaffed, lacked supplies and were often unable to provide critical care.
When Pedro Miguel was eventually admitted to the hospital, in addition to being severely malnourished he was found to have a heavy infestation of hook worms. The larvae of these parasites gain access to the body by penetrating the bare skin of the feet when they come in contact with dirt contaminated by feces of infested persons. Large numbers of hook worms in the intestine produce steady losses of protein and blood which, when combined with a meager potato and corn diet deficient in protein, results in classic kwashiorkor. Fortunately Pedro Miguel recovered well after receiving a transfusion of red blood cells (whole blood is not used because the heart is often weak in severely malnourished children and may “fail” if the volume of blood is rapidly expanded by transfusion) and a medicine to rid him of the hookworm. Over a period of two weeks the swelling disappeared, appetite returned and his mood improved.
When it was time to send him home the students realized the futility of their effort. To be sure, Pedro Miguel was given a pair of shoes, but he was not used to wearing them and probably would not wear them. In spite of the successful treatment Pedro Miguel was still poor and the circumstances leading to his illness had not changed. He was going back to his parents who even if more enlightened now were not better able to feed him a nourishing diet. He was returning to the same contaminated environment and to the same village destitute of medical care and even the most elementary of preventive services such as vaccination. But those problems were beyond the mandate of the medical establishment. A professor of Nutrition at the local University refused to lecture about protein/calorie malnutrition because he believed the subject belonged in Economics’ he felt that the medical profession contributed little to the control of this very important pandemic by “medicalizing” the problem and failing to consider its roots in poverty and marginality.
Children like Pedro Miguel do not grow well. If they reach adulthood, and many do not, they are shorter than less disadvantaged peers. Chronic hunger and each bout of infectious disease stunts their growth. The opportunity for catching up is denied to them by deficiency in the quality and quantity of diet available during convalescence. The prevalence of stunted children is a good proxy for the prevalence of the malnutrition-and-infection epidemic that still claims many lives in developing countries. Malnutrition contributes significantly to half of the deaths from diarrhea and respiratory infection and measles worldwide. The survivors are small in stature; they may look normal like those children surrounding Father Fernandez in the photograph, but they do not achieve normal growth and their capacity for learning is reduced. Their diets are deficient in more than calories and protein; iron, vitamin A and other essential nutrients are also likely to be in short supply. Malnourished mothers give birth to low birth-weight babies who are much more likely to die during infancy. In Latin America they are called victims of “el sindrome pluricarencial de la infancia ” or “multiple deficiencies syndrome of infancy”.
Fortunately the malnutrition-infection pandemic is waning world-wide. The World Health Organization reports a decline in stunting world wide (defined as the proportion of children who fall below 2 standard deviations below the mean of the reference standard population) from 47% in 1980 to 33% in 2000. In Latin America and the Caribbean the rate of stunting declined from 27% in 1980 to 17% in 2000. Urbanization, development, improvement in female literacy and access to adequate diets and basic health care in some of the Caribbean countries and South America partially explain this welcome trend. Unfortunately the prevalence of stunting has not declined significantly where large indigenous populations remain at the margin of economic development or where armed conflict victimizes everyone, particularly the poor. Between 1980 and 2000 the prevalence of stunting in Central America declined only from 26 to 24 percent. There are no easy cures. Programs that target only one of the many problems faced by poor rural families are likely to reap limited success. Empowering target populations through education, basic health care, infrastructure development and access to work with just remuneration are essential steps towards reducing extreme poverty, a prerequisite for access to an adequate diet. Progress has been made in the hemisphere but much remains to be done.
The new pandemic
The transition from rural to urban living which often translates into the transition from rural to urban poverty is at the root of a new world-wide pandemic of chronic diseases that has not spared Latin America or the Latin American diaspora in the United States. Juan Mario Vasquez a fifty year immigrant from Central America first came to the Spanish Clinic at Brigham and Women’s Hospital four years ago complaining of headaches and frequent urination, a possible symptom of diabetes. Both his blood pressure and blood sugar were high. Mr. Vasquez had come to the U.S. 15 years earlier at which time his lifestyle changed drastically. Instead of walking or riding his bicycle (he had been a bicycle racer in his youth) he now drove a car; his diet was rich in red meat and rice but sparse in vegetables, whole grains and fruit. He had learned to eat fast and had gained 30 lbs. He also felt he had little leisure. Cholesterol was borderline high. He was not an unusual patient in any primary care practice in the US. After a complete medical evaluation which did not show any heart problems, he was encouraged to eat more vegetables, black beans, fish, lean poultry, fruits, vegetable oil and whole grain breads while reducing as much as possible red meat, animal fat, sugar, potatoes and white rice. He was also “prescribed” a return to cycling while acknowledging the possible side effects: injury or worse inflicted by Boston drivers. It worked. One year later Mr. Vasquez’ blood pressure and blood glucose were normal without medication. He had lost 20 lbs and during the summer was averaging 90 miles per week on the bicycle.
Two years ago another patient, Felicio Valderrama, 46, developed fairly severe diabetes which required two different medications to control. He accepted as a challenge the recommendation to loose weight and exercise. He began walking, and later jogging, one hour a day, five days per week and lost 12 pounds. His blood sugar has been normal for almost two years and he no longer needs medications. Unfortunately such success stories are rare. Valderrama is a chef who understands food preparation. He has made his new diet enjoyable and finds it somewhat reminiscent of the diet of his youth. He also had a sport which he loved as a young man which he can still practice and enjoy. Valderrama likes running, he is proud of having controlled diabetes and happy to share his experience with others.
Acculturation entails dietary and other lifestyle changes that have important health consequences including the risk of developing what has been termed the “metabolic syndrome” or syndrome x: obesity, diabetes, hypertension and eventually heart disease. Societies in rapid transition appear more vulnerable to the metabolic syndrome. Two factors seem to be involved: genetic predisposition and a new lifestyle that includes calorie-dense diets, physical inactivity and aging. The genetic basis of the syndrome is complex and there is evidence that a number of genes may be involved resulting in heterogeneous biological processes that reduce the effectiveness of insulin. Native Americans are particularly at risk once they adopt the western diet and life-style. In the United States Native Americans, African Americans and Latinos are disproportionately affected. One of each 17 persons in the US has adult onset diabetes (may also have other components of the syndrome) but only half as many have been diagnosed. The prevalence of adult diabetes among Latinos in the US is over twice the prevalence among non-Hispanic whites: Twenty five percent of US Latinos are diabetic by age 45and 33% by age 65. Current projection are that by the year 2020 Latino and non Hispanic Blacks will account for 80% of the total increase in the number of diabetics between the ages of 20 and 70. As the Latino population ages the umber of diabetics will increase dramatically. Latinos are more likely to be diagnosed late and to have developed some complications by the time of diagnosis. A recent national survey (HAYNES III) showed that, once diagnosed, Latinos are less likely to be well controlled, thus increasing the likelihood of serious complications such as heart disease, blindness, amputation and renal failure requiring dialysis or kidney transplantation. Diabetes is enormously expensive to treat:15% of health care dollars are spent treating diagnosed diabetics who comprise 7% of the general population. Adult onset diabetes, and very likely the associated components of syndrome X, are becoming a very serious health problem worldwide. Diabetes is most prevalent in industrialized nations, the Middle East and Latin America and the Caribbean. The rate in Latin America is higher than would be expected, considering the level of economic development and degree of urbanization in the region.
In conclusion, a concerted effort is needed to continue to reduce protein energy malnutrition, particularly among children and pregnant women. Combating extreme poverty is the centerpiece of this endeavor since the vast majority of victims of protein-calorie malnutrition are the very poor and the very young in both rural and urban settings. Better education, infrastructure development and more equitable distribution of opportunity and income should be the goals. It is also urgent to control the emerging epidemic of chronic disease in Latin America. In the US, health care budgets are being strained by the use of high technology to treat the consequences of syndrome X: coronary artery disease and the complications of diabetes such as renal failure. Latin America cannot afford such expenditures. The challenge is prevention. It will require better understanding of the genetics of syndrome X. It will also require behavior change and a change in the new urban diet. We need to devise practical ways to counter the habit of sitting in front of televisions instead of keeping physically active. We need to engage educators, economists, anthropologists and urban planners in addition to health professionals to bring about change in the lifestyle of the new city dwellers. We need to increase access to a healthy diet, rooted perhaps in Latin American culinary traditions such as the one proposed by Oldways and summarized in the Latin American Diet Pyramid. Otherwise we risk going from the frying pan into the fire.
Spring/Summer 2001
Manuel Guillermo Herrera-Acena is a senior Lecturer on Nutrition, Harvard School of Public Health; a Lecturer at Harvard Medical School, and Director of the Spanish Clinic, Brigham and Women’s Hospital.
Related Articles
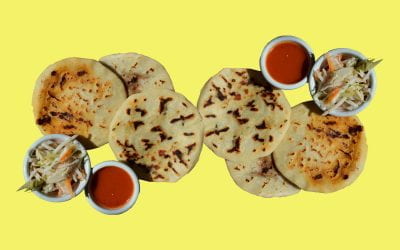
Salvadoran Pupusas
There are different brands of tortilla flour to make the dough. MASECA, which can be found in most large supermarkets in the international section, is one of them but there are others. Follow…
Salpicón Nicaragüense
Nicaraguan salpicón is one of the defining dishes of present-day Nicaraguan cuisine and yet it is unlike anything else that goes by the name of salpicón. Rather, it is an entire menu revolving…
The Lonely Griller
As “a visitor whose days were numbered” in Buenos Aires, Argentina, he tossed aside dietary restrictions to experience the enormous variety of meat dishes, cuts of meat he hadn’t seen…