Safe Blood for Transfusion
The Challenge of Scarcity
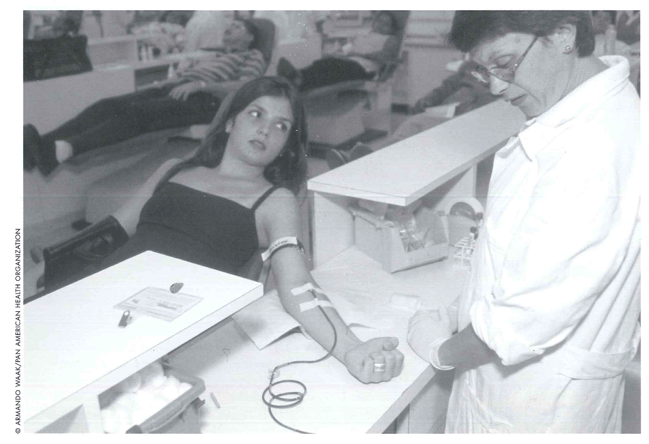
A young woman gives blood in a clinic. Blood for transfusion is scarce in all coun- tries in Latin America and the Caribbean.
José Oscar Cotto López has donated 140 pints of blood since 1966. The 53-year old resident of San Salvador, El Salvador, does so because he believes it is an expression of love. “We must be aware that donating blood is the best way to express solidarity and love to our fellow human beings,” he says. “It is the most beautiful gift we can give, the gift of life.”
Unfortunately for the people of the Americas, Cotto López is a rare individual. Blood for transfusion is scarce in all countries of the Americas. Only Cuba collects blood from the equivalent of five percent of its population, the amount that the World Health Organization and the International Federation of Red Cross and Red Crescent Societies estimate is necessary for a community to achieve sufficiency. Most of the remaining countries hardly collect one-fifth of what they need.
Due to the scarcity of donors, hospital-based blood banks in Latin America usually ask patients’ relatives to bring in two or three blood donors known as replacement donors to cover the patient’s needs. Sometimes, relatives have difficulty finding people who will donate blood and must resort to buying it. In other instances, the blood bank itself pays the “donor.”
Working with the Pan American Health Organization in laboratory and blood services all over the region, I have found that replacement and remunerated donors usually do not respond to pre-donation questionnaires with honesty,. They need the monetary incentive or feel they are being forced into giving blood, so they hide risk behaviors from the blood bank personnel. “I don’t even bother asking the donors all those questions; they all lie,” a nurse in Santiago, Dominican Republic, told me. “We take a blood sample from the potential donor early in the morning, test it for infectious markers and, if the results are negative, we draw his blood later that day,” said another nurse in Mazatenango, Guatemala.
Practices like these increase the cost of the blood collection process and represent a serious hurdle for ensuring the safety of blood in the Americas. For example, Dr. Marco Herdoiza, Secretary of Ecuador’s Blood Program, found that , in 1998, the probability of finding a donor with a positive marker for hepatitis B, hepatitis C or HIV/AIDS is 12,000 times higher in blood banks that collect all their blood from replacement donors, than those that have at least 60 percent voluntary, altruistic, non-remunerated blood donors.
Programs to promote voluntary, altruistic, non-remunerated donations are practically nonexistent in the Latin America and the Caribbean. In a few countries, the Red Cross blood bank may have a mobile team — with both personnel and a vehicle — that collects blood from donors in either their workplace, or in social and religious centers. But these are, for the most part, unusual. “The only place I see posters asking people to donate blood is the blood bank,” said a young woman in Managua, Nicaragua. “Why don’t you place them in supermarkets, movie theaters or shopping malls?”
A common belief in all Latin American countries is that donating blood makes a person either gain or lose weight. Others believe that giving blood is literally an act of giving away the essence of life. An individual in Quito, Ecuador, put it this way: “I am not going to give part of my life away. they tell me that by giving blood I also give life.”
We must develop and implement structured social marketing and educational programs aimed at recruiting donors from the population groups that are at low risk of acquiring and transmitting infectious diseases.
The safest blood donors are the voluntary donors who give blood repeatedly. And first-time donors will come back voluntarily only if they receive adequate information and proper treatment from the blood bank personnel. Therefore, blood banks must be accessible and donor-friendly. “It is hard to get to the hospital and, once in the hospital, it is difficult to find the blood bank,” a potential donor in Guatemala City commented. In addition, the infrastructure of the blood banks must be improved. “I not only give my blood and my time, but also must buy the bag to collect my blood,” complained a donor in Asunción, Paraguay.
Attitudes of blood bank staff sometimes aggravate these problems. If blood donors express mistaken beliefs and common myths, blood bank personnel often will treat donors as ignorant. Very seldom will they try to educate them. In fact, more often than not, personnel who interview the potential donors seem to be looking for ways to catch them telling untruths about potentially risky behaviors.
Furthermore — and associated with the lack of harmonized, structured questionnaires and the lack of continued in-service training — staff may miss the point of the interview. On various occasions when I pretended to be a donor, I was turned down because I had just traveled, even though the country I had just traveled from was the United States. Or my age became a question. I was told that in the absence of clear guidelines the blood bank would defer anybody who was “too old.” When I asked the nurse to explain what “too old” meant, she responded, “Anybody over 50.” So I responded, “In that case, I could not give blood” because I was 51. Obviously embarrassed, the nurse told me, “You don’t look 50, you can donate.” It is clear to us, then, that programs to promote voluntary, repeated, altruistic, non-remunerated blood donation must include an educational component directed at blood bank staff.
With the support of a group of anthropologists, the Pan American Health Organization has developed the “Methodological Guidelines for Socio-Cultural Studies on Issues Related to Blood Donation.” These guidelines have been adapted for local application in El Salvador, Nicaragua, Dominican Republic, Colombia, Ecuador, Argentina and Paraguay.
The research has been used to develop the content of public service announcements taped by Don Francisco the host of the popular weekly show “Sabado Gigante,” broadcast from Miami to 30 countries. Don Francisco Mario Kruesberger in real life — has accepted the task of being the messenger for PAHO’s appeal to the Latin American countries on voluntary blood donation issues. PAHO is also helping national blood authorities develop their own programs, with social marketing as a very strong component.
We are supporting the in-service training of blood bank personnel, using the distance learning approach. Modules on “Safe Blood and Safe Blood Products” have been developed by the World Health Organization and translated into Spanish by the Asociación Argentina de Hemoterapia e Inmunohematología. Specific programs in academic centers or by health authorities in Mexico, El Salvador, Honduras, Nicaragua, Colombia, Ecuador, Peru, Paraguay, Uruguay, Argentina, Dominican Republic are now using these modules.
To date, more than 5,000 professionals and technicians have initiated the distance learning program on safe blood and safe blood products in Latin America. We expect that with the active participation of the University of West Indies the modules will by applied shortly in the English-speaking Caribbean.
The availability of mobile teams that can collect blood in workplaces, social clubs, churches or other public places is also very important. In addition, they must have adequate resources, including personnel and budget. We believe that the collection of blood for transfusions should be taken out of the hospital environment. If blood banks are accessible to the public, friendly to the donor and properly staffed, they will contribute greatly to voluntary, repeated altruistic donation.
Fall 2000
José Ramiro Cruz received his degree of Master of Science (1976) and his degree of Doctor of Science in Virology and Immunology (1980) from the Department of Tropical Public Health, Harvard School of Public Health. He is a regional advisor, laboratory and blood services, for the Pan American Health Organization
Related Articles
Latino Mental Health
What brings you in to see me today?” This is the typical question asked of new patients during a psychiatric evaluation in a Boston clinic. When asked of a Latino patient, however, the answer…
Health: the Hope of Haiti
At no time have I felt more vital than in serving at Partners In Health (PIH), and seldom more needed than in places like Haiti. In the Haitian people, as well as in every other country that PIH serves, we find an…
Whither Equity in Health?
A waiting room in a charity clinic in rural Haiti. It is a humid afternoon, and huge drops of warm rain are starting to fall. A young woman is watching as her ten-year-old son, Dominique, clutches…