Whither Equity in Health?
The State of the Poor in Latin America
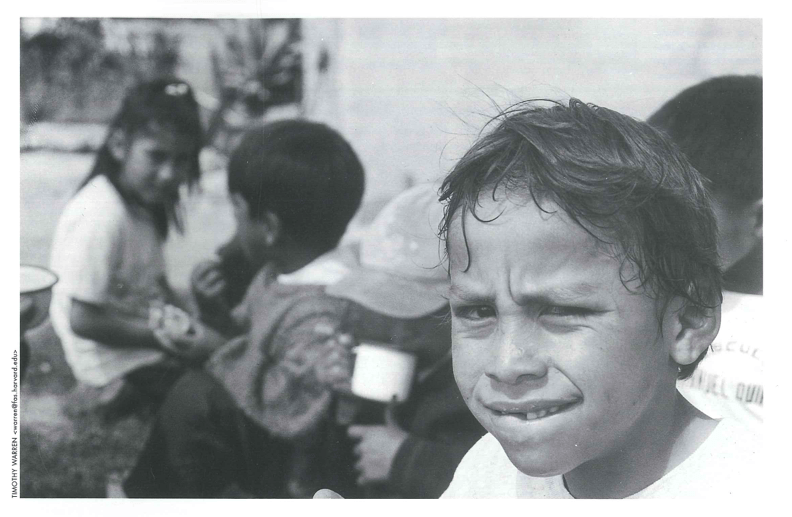
Schoolchildren in Tumbaco, Ecuador, enjoy a nutritious breakfast provided by UNICEF
A waiting room in a charity clinic in rural Haiti. It is a humid afternoon, and huge drops of warm rain are starting to fall. A young woman is watching as her ten-year-old son, Dominique, clutches miserably at his abdomen; he is staring at the roof, not saying anything. A Haitian colleague says to me, “His temp is 104, it’s been up for over a week, his belly pain began three days ago. I’m getting the films and labs now.” He pauses, looks darkly at the mother: “It’s late.” I say nothing, but look at the woman as I reach for the boy’s abdomen, praying that it’s not yet rigid (it is not). Though she is no doubt younger than I, she appears weathered, for Haiti has been no kinder to her than to her son. She looks at me, sighs, and wordlessly makes a weary gesture. I know it well: What can I do, she asks with her hands. It’s beyond my control.
And so it is. Well beyond her control. Her boy probably has typhoid fever, and the severe abdominal pain is ominous: one of the worst complications of typhoid is intestinal perforation, which usually leads to peritonitis and death in rural Haiti. Typhoid, a classic public-health problem, is caused when drinking water is polluted by human feces. Not her fault. Ours perhaps, I think immediately. We could have worked harder on water-protection efforts, even though another, more conventional voice in my head reminds me that Dominique and his mother live well outside of our “catchment area,” the region in which we. Partners In Health, a Harvard-affiliated public charity work closely with community-health workers. And only by redefining the whole of public health as a private concern, one to be handled by do-gooder organizations like our own, could this be seen as our responsibility.
Increasingly, such a redefinition the “privatization” of health has come to hold sway in the hemisphere. Assessing public health in Latin America is a treacherous exercise. This is not because it is impossible to evaluate the state of the region’s health, nor is it because the admittedly enormous variation, both across and within nations, leads to analytic impasse. It is treacherous to comment on public health in Latin America because of the ideological minefields one has to traverse in order to do so.
In the past, such assessments may have been easier, and not because public health was then a more robust undertaking. Rather, there was formerly a consensus that the health of the poor meaning people like Dominique and his family was a cardinal indicator of how well the stewards of the public’s well-being were doing their job. Rudolph Virchow has been called the father of social medicine, and it was he who termed doctors “the natural attorneys of the poor.” Doctors were supposed to defend the poor because the impact of their social condition poverty was embodied as preventable or treatable sickness.
As public health has become a larger enterprise, it has defined a turf of its own; as nation states have come into being in Latin America, they have defined national public-health agendas, increasingly with the assistance of international experts. The “welfare state” that we think of as having been progressively built up, from the 1930s to the beginning of its decay in the 1980s, barely got a start in Latin America before debt, the cupidity of local strongmen, and the agenda-setting of First World economic advisers attempted to terminate it as a public responsibility. The health of the poor is now deemed less important than what is often termed “cost-effectiveness,” which too often calls for minimizing the drain on national budgets increasingly dedicated to the supposedly higher goals of debt service and privatization.
Those struggling to promote the health of the hemisphere’s poor are now in the defensive position of having to show that proposed interventions are both effective and inexpensive, regardless of gravity of the health problem in question. Some would be surprised to learn that the largest financiers of public health in Latin America include the international financial institutions, such as the World Bank and, less directly, the International Monetary Fund. In some regards, this makes sense, given the undeniable association between economics and health. But there is a dark side to the new accounting, as even a physician can see: such sources of funding for public health place us within a framework developed by economists working within a paradigm in which market forces alone are expected to solve social problems. As efforts are made to determine whether or not an intervention is “cost-effective,” the destitute sick are often left out altogether.
As time has gone by, certain trends have become palpable within much of Latin America. Some have been favorable: vaccination and other interventions have lowered infant mortality; polio has been eradicated from Latin America. Some countries, such as Chile and Cuba, have health indices similar to those registered in North America. But in most of Latin America, we see that a shrinking commitment to public subvention of health care and a push for its privatization have led to a widening gap in access to quality health care. These trends are registered even as the fruits of science become ever more readily translated into effective therapies. And that, in my view, is the central irony of public health in Latin America: national statistics continue to suggest improvement, even here in Haiti. But the poor, as Dominique’s experience suggests, are doing poorly. They are doing a bit better than in previous decades, but much less better than might be expected, if the fruits of science and technology were used wisely and equitably.
It has been my great privilege to spend most of my adult life working as a doctor in Latin America, including many working visits to Peru and Mexico. But the country I know best, although it is sandwiched between two indisputably Latin countries, is one often forgotten in Latin American studies. When I first went to Haiti, in 1983, I remember writing “West Indies” at the end of my Port-au-Prince return address. I stopped doing this after reading a multi-volume history of the U.S. military occupation of Haiti (1915-1934). The author, Roger Gaillard, had affixed his address to the inside of each volume. After Port-au-Prince, Haiti, he added “Amérique Latine.”
It was a polemic note, perhaps, but Gaillard had a point. Haiti is, in many ways, the most “Latin American” of all countries not because it is “Latin” in having a Romance-based Creole for its national language, and not because of its historical Catholicism, but because of its having endured a history the outlines of which are familiar throughout South and Central America. When we look back at mid-century writings about the region, we find political scientists describing Latin America as poor, rural and agrarian; as having high indices of social inequality; as marked by colonialism (once European, now a condition described as being in the “sphere of influence” of the United States). On each of these counts, the most extreme example is Haiti. One of the reasons Haiti has become so Latin American is that it has had more time to do so. Haiti is the oldest republic in Latin America, independent (at least in name) since 1804. When Simon Bolivar was looking for allies and supplies, he went to Haiti, which welcomed and supplied him.

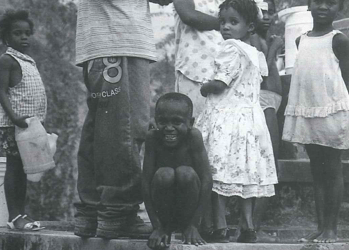
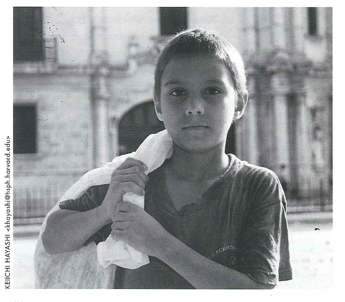
The health of the poor – like this young boy in Haiti – is now deemed less important than cost-effectiveness.
Although Latin America has changed enormously since mid-century, there is a part of every Latin American country that has much in common with Haiti. A trip to a poor village in Chiapas or highland Guatemala reminds one of Haiti far more than might a trip to the French overseas départements of Guadeloupe and Martinique. Political violence, among other afflictions of poverty, is endemic here. Haiti is the sickest of New World republics. (I am writing this essay in our clinic, between emergencies.) The history of Haiti’s poverty how it was generated and sustained is important, though often forgotten. If you are interested in public health, which you necessarily are if you are sitting in a clinic in rural Haiti, you cannot forget poverty’s impact on the Haitian people. This year, we are likely to see 45,000 patients in the ambulatory clinic as many as will be seen in the emergency room of Boston’s Brigham and Women’s Hospital, where I also have the good fortune to work. The difference, of course, is that the Brigham has a huge medical and nursing staff, excellent laboratories and radiographic services, operating rooms and blood banks, is located in the middle of a region dedicated to advanced medical research, and so forth. And apart from the fact that we don’t have such amenities here in Haiti, the patients are sicker. They come to us with illnesses such as tuberculosis, hypertension, malaria, dysentery, complications of HIV infection, all typically in a more advanced state than we’d see at the Brigham. The children are malnourished, and many of them will have severe protein-calorie malnutrition as well as an infection. Some will have typhoid, measles, tetanus, or diphtheria (although these patients will be, like Dominique, from outside of our catchment area). Some will have surgical emergencies: abscesses, infections in the chest cavity, fractures, gunshot and machete wounds.
Or they will be pregnant and sick. Few things are more tragic than third-trimester catastrophes: eclampsia, arrested labor, hemorrhage. As I write these lines, the local “midwives” are meeting outside. They’re not really midwives, they’re traditional birth attendants a mix of women and men, most of them over 50 and unable to read. None know how to gauge blood pressure. Many feel overwhelmed. And justifiably so. Maternal mortality is higher in Haiti than anywhere else in Latin America. In one study, conducted a decade ago around the town of Jacmel in southern Haiti, maternal mortality was 1400 per 100,000 live births. It’s under 20 in Cuba, Jamaica, St. Lucia, and the United States. Our clinic’s obstetrician-gynecologist long ago left for Florida, where he joined a community of more Haitian physicians than are now present in all of rural Haiti.
Seeing the rest of Latin America through Haitian eyes and, concurrently, coming to see Haiti as a Latin American country is an instructive exercise. When I first went to Mexico it was on a visit to the national school of public health, in beautiful Cuernavaca. This looks nothing like Haiti, I thought. Then I started visiting Chiapas, and had something with which to compare both Haiti and Cuernavaca. I was at first surprised to see that parts of Puerto Rico looked so much like Florida, where I had grown up, and this reversal of expectations. I’d thought that the Caribbean islands would look more alike led me to read more about the history of colonialism in the region, and to seek to understand more about the flow of people into and out of the Caribbean. Peru was another eye-opener: although significantly less poor than Haiti, the slums of northern Lima recalled the dusty towns of northwest Haiti. And here was a place where my Haitian clinical experience proved helpful: in the Peruvian shantytown of Carabayllo, rates of tuberculosis were as high as in Haiti as high as anywhere in Latin America. What’s more, disruptions in the economies of these countries were felt immediately among the people who were my hosts in each of these settings. As in Haiti, the poor felt the impact of adverse trends before any others; their health suffered, often grievously.
Keiichi Hayashi made this photo of a boy in Havana, Cuba, during a Harvard School of Public Health study tour.
Haiti is often compared, and unfavorably, to the Dominican Republic. Neither country has much to boast about in terms of public health. The country sited on the other two-thirds of the island has poor health indices, if nowhere near as bad as those here in Haiti. But what about Haiti’s second-closest neighbor? Although popular conceptions in the United States sometimes underscore similarities between Haiti and Cuba one generates boat people, the other balseros one could not find a starker contrast within this hemisphere. There are some similarities in initial conditions: less than 100 miles apart, the two islands have identical climates and topography. And like Haiti, Cuba has known major economic disruption in the past decade. The impact on Cuba of the breakup of the Soviet Union, which contained its major trading partners, has been much commented upon. From 1989 onward, the Miami papers have been full of predictions of the imminent fall of Castro and the end of communism in Cuba. But in fact Cuba, unlike Haiti or Chiapas or Peru, has not known significant unrest or political violence.
The Cuban economy, however, did sustain major blows. I’m no economist and some might argue that it’s even more difficult, in economics, to wade through the ideology than it is in public health but reports suggest a net loss, between 1989 and 1994, of more than 80% of all of Cuba’s foreign trade. This was as severe a contraction as that faced by any Latin American economy. So what about the impact of such seismic rumblings on the health of the Cuban poor? Was the story the same as in Haiti (or Peru or Chiapas), where economic turmoil led inevitably to immediate and adverse impacts on the health of the most exposed part of the population? The short answer: no. In fact, although much is made of the harm done by the U.S. embargo to Cuban medicine, the Cuban people remain healthy. Even epidemic optic neuropathy, locally and internationally attributed to vitamin deficiency, was more likely caused by an as yet unidentified viral pathogen.
Some years ago I turned, with fascination and a bit of dread, to comparing these two neighbors. Haiti has the highest maternal mortality in the hemisphere; Cuba’s is among the lowest. Haiti has the highest infant mortality rate in the hemisphere; Cuba, the lowest (in fact, infant mortality in Mission Hill, mere yards from the front door of the Brigham and Women’s Hospital, is said to compare unfavorably to Cuba). The leading killers of young adults in Haiti are tuberculosis and HIV; Cuba has the lowest prevalence of HIV in the hemisphere, and remarkably little tuberculosis. Typhoid, measles, diphtheria, dysentery, dengue, parasitic infestations all are common in Haiti and almost unknown in Cuba. I could rattle off any number of indices leading to the same contrasts. There’s a saying in Cuba: “We live like the poor, but we die like the rich.”
In Haiti, as in Chiapas and the slums of Lima, poor people live and die like poor people. They die of preventable or treatable infections; they die of violence. Why, then, do Cubans leave Cuba? One of the reasons is probably that poor people are not satisfied to die like rich people, they want to live like them, too. This is for me a philosophical question rather than a medical one; I have not interviewed poor people who die of the same diseases that end affluent lives in their eighth decade. The people who crowd our waiting rooms here in Haiti do not have such expectations; they do not have such life expectancies.
I recently went to visit the new Escuela de Medicina de las Americas, with which Cuba proposes to serve the hemisphere by training a new generation of doctors. Say what you will about propagandistic intent, transforming- in less than a year- a naval base into an international medical school is the ultimate in swords-into-plowshares. The facility was attractive and clean. There were few supplies, of course, and not much in the way of textbooks. But the student body came from all over Latin America. And they looked quite different from the students I had met in the capital cities of the region. Several of the students from Bolivia, Mexico, and even Colombia had the look of indigenous people, the ones you could imagine seeing scorned for their appearance or their accent in the streets of La Paz or San Cristobal de las Casas.
I was there to beg for medical school spots for rural Haitians, of course, and the Cubans were more than interested. My tour guide was none other than Dr. José Miyar, a Secretary of State and one of the leading figures in the development of Cuba’s health sector after the revolution. We spoke about Haiti and other countries with similar health indices. “Maternal mortality” commented the white-haired doctor, looking pained. “Not merely a tragedy in itself, but the cause of a long chain of tragedies for the other children who survive. For then comes malnutrition, diarrhea, and, often enough, death for these children.”
Maternal mortality brings me back from pleasant memories; I am not visiting Cuba this morning, but opening office hours in Haiti, the place I call home. There is a long line in front of the women’s health clinic. We’re hoping to recruit a new obstetrician-gynecologist. We’re also in need of a pediatrician. We’ve had offers from U.S. physicians, but need fluent Creole speakers. The operating room is closed for a while, as we await the arrival of a full-time surgeon. She is Cuban.
Outside, I hear the midwives chattering. When they talk to me, they speak of their own ailments. “How can I walk to deliver babies when my leg hurts so much?” queries one. Another adds, “We are hungry and do not have gloves or aprons.”
Definitely back in Haiti.
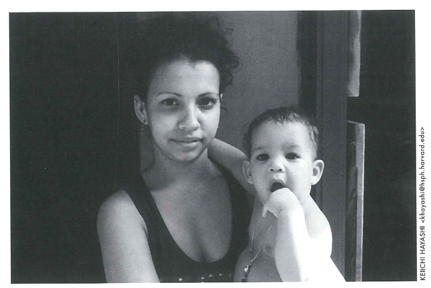
A mother and child in Cuba. For a complete account of the Har- vard School of Public Health study tour, see chttp://www.fas. harvard.edu/~drclas>
At the close of June, 2000, the World Health Organization released an assessment of the health systems of all member states. The evaluation took into account several indicators, including quality of health services; overall level of health; health disparities; and the nature of health-system financing. Of 191 countries surveyed, the United States spent the highest portion of its gross domestic product on health, but ranked only 37th in terms of overall performance. Tiny Cuba, spending a smaller portion of its small GDP, was ranked at roughly the same level as the United States, and was one of the four highest-ranked countries in Latin America. As for “fairest mechanism of health system financing,” Cuba was the number one nation in Latin America; in this category, the United States did not even figure in the top 50.
What conclusions can be drawn from these comparisons? Audiences in the United States, I have found, are not pleased to hear such analyses. But if they are revealing and startling, surely there is some point in discussing them? I know that I’m not so much interested in the ideological underpinnings of the various approaches to public health as I am in the results, as manifest in morbidity and mortality rates. Let the editorialists rant about socialism or its opposites; doctors and public-health practitioners have to be “outcome-oriented.” Of course, the major debate in social policy is about what outcomes should be perceived as “of interest.” For economists, such matters as GNP and external debt are the preferred indices (although these are, in my view, ideologically freighted subjects in and of themselves). For education experts, it’s literacy rates. The human rights community, interestingly, almost always narrows its focus to privilege rights of expression and representation and to exclude social and economic rights an omission that should trouble physicians, who need supplies of tangible goods, the very tools of their trade, before they can go to work. Unless the Latin American poor are accorded some right to health care, water, food, and education, their rights will be violated in precisely the ways manifest in my waiting room here in Haiti: their lives will be short, desperate and unfree.
Just ask the Cuban doctors now working here. There are probably more Cuban physicans in rural Haiti than there are Haitian doctors (remember: the Haitian M.D.s are in Port-au-Prince, Florida, New York, Montreal, et cetera). What do the Cubans do when they encounter patients so poor that they cannot fill prescriptions, buy intravenous solutions, or feed their children? The Cubans are well-trained, clearly, and skilled at making the most of scanty resources. But all the training in the world cannot substitute for a healthcare system. They, too, will have to start from scratch and learn to beg for supplies, as we all do down here if they wish to serve the Haitian poor.
And so I return, as always, to the health of the poor as the most telling social-policy outcome. Even as national economies and stock markets boom, the health of the Latin American poor remains abysmal by both absolute and relative criteria. This is true in Chile, Brazil, Mexico, Peru and of course Haiti. It’s a quick enough trip from the glittering towers of Mexico’s zona rosa to the squalid villages of Chiapas. In Lima, excellent highways lead past glass bank and insurance skyscrapers to the miserable invasiones of the city’s northern reaches, where, as noted, rates of tuberculosis run as high as anywhere in Latin America. The shiny towers and dismal health statistics are of course related, since the privatization of health care occurs at the same time, and as part of the same policy environment, as do massive transfers of public wealth to private coffers. This year, Peru will pay about 20% of its GNP to finance its foreign debt. Most of it will go to even taller towers in wealthy cities like New York. Even well-off Chile, with three times the per capita income of Cuba, has been forced to acknowledge a growing equity gap in health outcomes.
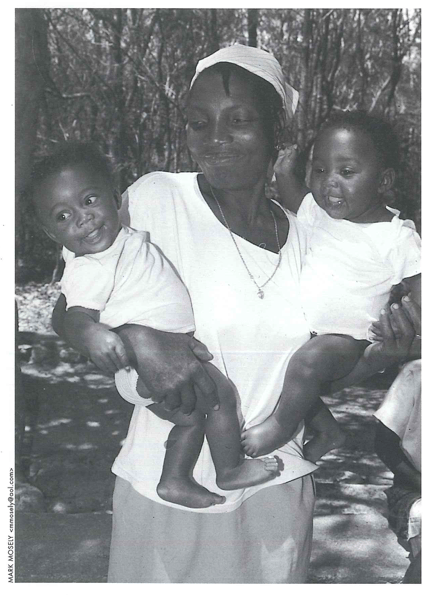
Haitian mother waits with children for immunizations.
Watching the health of the poor is the best way to assess public health in Latin America, but these days there is more enthusiasm for “environmental report cards” than for this once-respected marker. Indeed, the rain forests and their non-human fauna seem to occasion more comment than the premature deaths of the hemisphere’s poor. The poor in most poor countries are living in the worst of the industrial world’s off-scourings, surrounded by bad air, bad water, bad soil, and working, when they can find jobs, under dangerous conditions; but it is a rare First World environmentalist who recognizes them as deserving to be “saved” no less than the forests, the whales and the tree frogs.
Back to our waiting room. What is to be done if we want to take stock of the health of Latin America’s poor, and act purposefully? Of course, we need resources, and to be quite honest, resources should not be the problem. In this time of record profits for many industries and dazzling individual fortunes, is it unthinkable that we should spread the wealth? I just came across an interview with the chairman of Intel, a certain Andy Grove. He grew up in Hungary, he notes, during the Stalinist era. “Profits are the lifeblood of enterprise,” he remarks. “Don’t let anyone tell you different.”
Unlikely that anyone would try, these days. Certainly not a physician sitting in a clinic in rural Haiti. But surely there is some way to redirect some part of the profit stream to take care of the destitute sick, right now? Otherwise, doctors will stand by, as helpless as Dominique’s dispirited mother, watching resources flow along the gradient established for them by our policies, our choices, and our blind spots to become ever more narrowly concentrated in the hands of a few. If the health of the poor is the yardstick by which our public-health efforts in Latin America are judged, we or our descendants will have a lot of explaining to do when history sits to consider our case.
Fall 2000
Paul Farmer, MD, PhD, is a medical anthropologist whose work draws primarily on active clinical practice: he divides his clinical time between the Brigham and Women’s Hospital (Division of Infectious Disease) and a small hospital in rural Haiti. Through Partners In Health, the public charity he helped to found, his work has focused on the prevention and treatment of diseases disproportionately afflicting the poor. The Program in Infectious Disease and Social Change, which Farmer runs along with his colleagues in the Department of Social Medicine, has pioneered novel, community-based treatment strategies for sexually transmitted infections (including HIV), drug resistant typhoid, and tuberculosis in resource-poor settings.
Related Articles
Latino Mental Health
What brings you in to see me today?” This is the typical question asked of new patients during a psychiatric evaluation in a Boston clinic. When asked of a Latino patient, however, the answer…
Health: the Hope of Haiti
At no time have I felt more vital than in serving at Partners In Health (PIH), and seldom more needed than in places like Haiti. In the Haitian people, as well as in every other country that PIH serves, we find an…
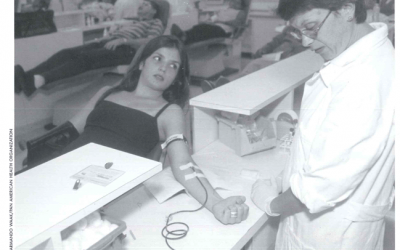
Safe Blood for Transfusion
José Oscar Cotto López has donated 140 pints of blood since 1966. The 53-year old resident of San Salvador, El Salvador, does so because he believes it is an expression of love. “We must be…